Running a behavioral health setup takes a lot out of people. Each day feels different. Sometimes you manage to keep up with everything, other times the work never seems to end. Staff sit with patients, write notes and try to keep files straight while billing piles up in the background. Even when the team gives their best, claims still get denied because of small mistakes. One wrong code or missing detail can slow the entire payment process.
The stress from slow claims builds up. Leaders worry about money. Staff feel overworked. Patients get stuck waiting while their records bounce back and forth. It is not fair to anyone. That is why speed and accuracy matter so much. An AI based Behavioral Health chart audit tool can step in here, handling the messy side of billing so staff save time and keep their sanity.
Why Speed Matters in Behavioral Health Claims
Late claims payments cause a ripple effect. Staff still need paychecks. Rent and utility bills never pause. Supplies keep running out. When claims take weeks or months, it becomes difficult to keep the whole place steady. It affects both staff performance and the quality of care.
Faster claims remove a lot of that pressure. Cash flow stays smooth, staff stop worrying about bills and leaders can focus on planning instead of chasing payments. Patients also notice the difference. They see fewer billing problems and trust grows. It is not only about the money, it is about peace of mind.
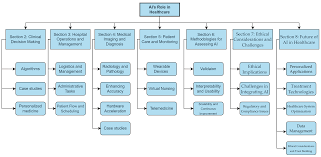
The Role of an AI Based Behavioral Health Chart Audit Tool
An AI based Behavioral Health chart audit tool helps clean up the process before problems start. It reviews records in real time. It checks codes, notes and other small details that humans often miss when the workload gets heavy. Instead of staff spending long hours fixing mistakes after denials, the tool points out errors right away.
This means claims leave the office cleaner and faster. Staff feel less overwhelmed. They know the tool is catching issues that would have taken hours to track down by hand. Patients benefit too, since their records move smoothly without the constant stops and delays.
How It Speeds Up Claims Processing
Claims often slow down because errors go unnoticed. A missed digit, wrong code or missing note can create weeks of delay. An AI based Behavioral Health chart audit tool spots these things before submission. This makes the back and forth with payers shorter.
Automated checks take some of the pressure off when it comes to staying compliant. Insurance companies want clean records and they look closely at every little detail. This tool helps staff keep claims in line with those rules. Fewer rejections happen and payments move faster. The revenue cycle stays steady and everyone feels less stressed. Staff gain confidence knowing they are sending in cleaner claims.
The Impact on Both Sides
Once billing starts going wrong, you can feel the tension in the air. Staff and patients both notice it. Staff feel drained from fixing errors. Patients get frustrated when they see mistakes on their bills. It pulls in both sides and keeps them in a loop that wears people down.
With automated audits, that cycle changes. Staff get back their time. They can spend more of it with patients and less with paperwork. Patients also see smoother billing. They no longer fear surprise costs or confusing errors. Denials are not rare either. A study found that about 17% of Medicare Advantage claims were denied at first, which shows how often patients get stuck in the middle.
Why Centers Should Consider This Tool
Running a behavioral health service means always juggling heavy work. Staff try to keep up but time runs short and errors happen. An AI based Behavioral Health chart audit tool takes over the repetitive checks that usually drain energy. It helps staff breathe a little easier.
The financial side also improves. Faster payments mean leaders can reinvest money into staff training, new resources or expanding services. A tool that fixes paperwork issues does more than speed up claims. It creates long term stability. That stability allows the entire service to grow stronger.
Key Benefits Beyond Claims
The benefits reach beyond billing. Better audits improve overall documentation. Everything stays more organized, with records updated and waiting for when a review is needed. Staff do not panic during audits or inspections. Everything is already in order.
This also makes handoffs between providers easier. With accurate notes and codes, teams communicate better. Patients move from one provider to another without confusion or repeating their story. The system helps create smoother teamwork across the board.
Building Confidence in the System
Trust is fragile in behavioral health. Patients need to trust their providers. Staff need to trust that the system supports them. Leaders need to trust that finances are stable. An AI based Behavioral Health chart audit tool helps build that trust. It takes away the fear of constant denials and shows staff they have backup.
Confidence spreads quickly. Staff feel lighter and more motivated. Patients see fewer billing issues. Leaders notice healthier finances. Everyone benefits when the system feels reliable. That sense of security strengthens the whole foundation.
Final Thoughts
Paperwork should not drain all the energy from behavioral health staff. Smarter tools are here to help. Smarter tools can take some of the weight off. An AI based Behavioral Health chart audit tool cuts down mistakes, helps claims move faster and gives staff a bit of breathing space.
When claims run smoother, staff get back time they usually lose on paperwork. That time goes back into care. Patients enjoy smoother experiences. Leaders see stable finances. The entire system functions better. Technology does not replace care but it supports it. And when support is strong, care only gets stronger.